A Blueprint for Optimizing In-Network Specialist Referrals
Understanding the Specialist Referral Value Chain
-
REQUEST THE FULL BUSINESS CASE
-
GET A DETAILED FINANCIAL MODEL
A Playbook for Increasing the Value of In-Network Referrals
White Paper
Understand the referral value chain and explore strategies to unlock downstream revenue.
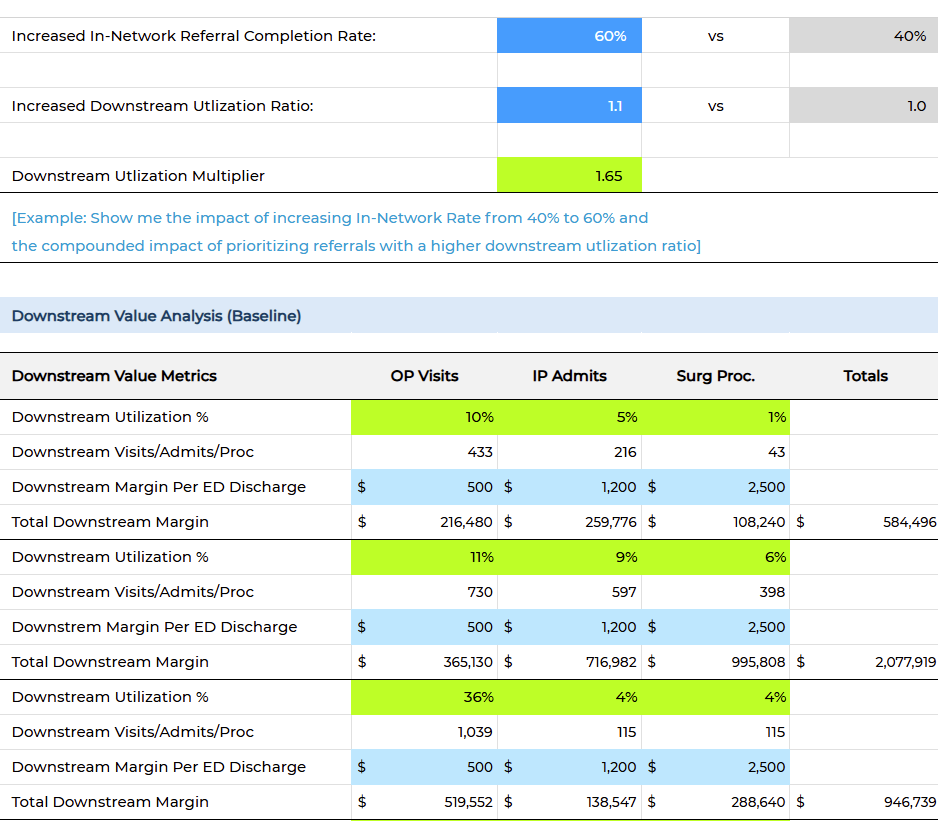
Financial Model
An interactive Excel model that shows the key metrics, calculations and underlying assumptions. Calculate downstream revenue potential for key service lines.
Infographics
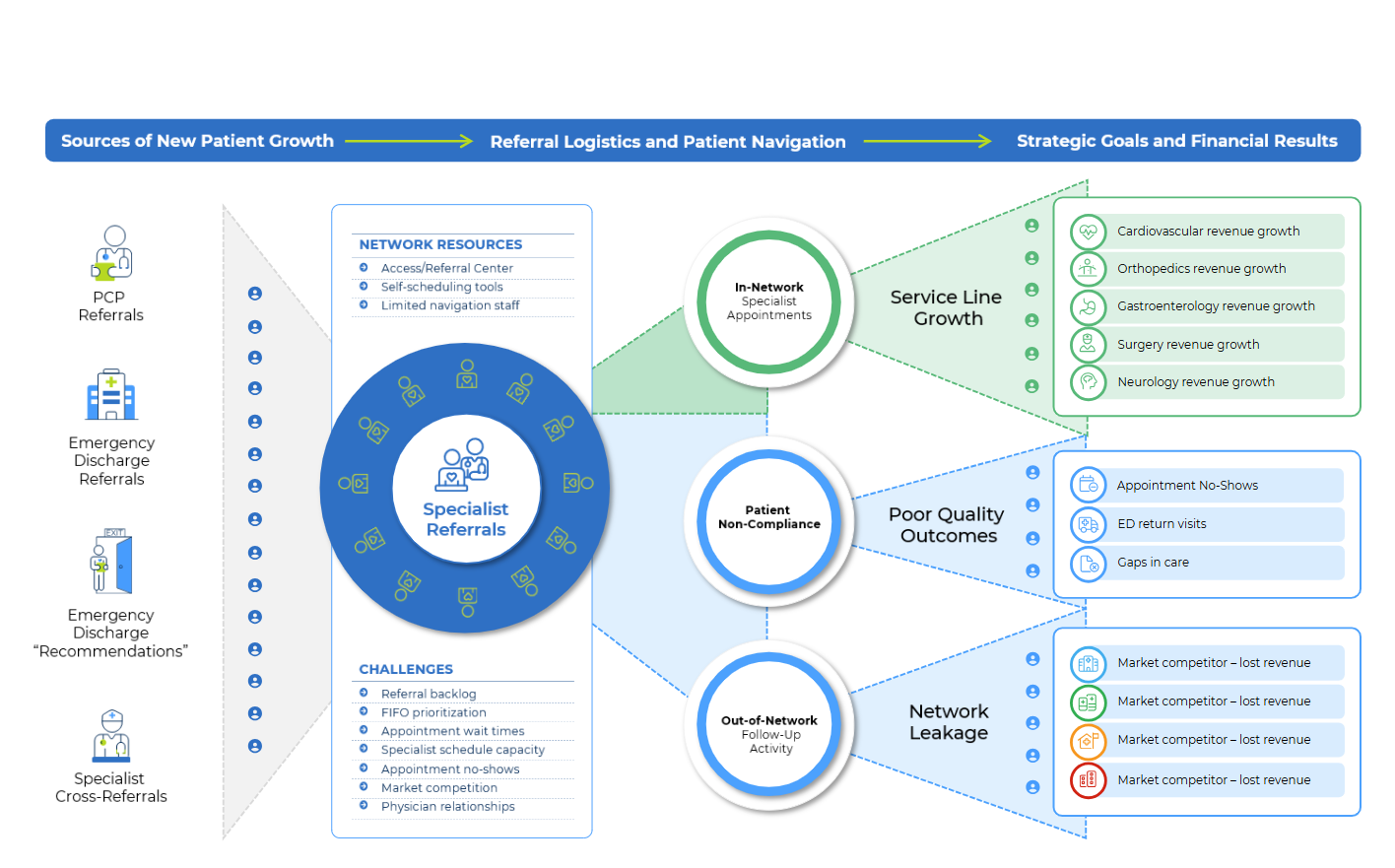
Workflow diagrams showing the sources of specialist referrals and the challenges navigating those patients to in-network appointments. Follow the flow of referrals as they are converted to service line revenue, quality outcomes or network leakage to competitors.
SIGN UP FOR EXCLUSIVE ACCESS
"One reason it can be difficult to analyze and improve the referral value chain is that it crosses over multiple health system functions and stakeholders. From the referral capture process in the ED and PCP offices, to the centralized Patient Access team, to the Medical Group specialist offices, to downstream procedures delivered in the hospital, to the strategy team analyzing network leakage – there is no one owner of this problem."
Network Leakage and Missed Downstream Revenue
-
Missing referral orders in the ED
-
First-In-First-Out (FIFO) prioritization
-
Self-scheduling yields low-value patients
-
Appointment no-shows waste valuable slots
-
Overburdened office scheduling staff
-
Limited visibility into referral patterns
Keep High-Value Referrals Attached to Service Line Growth
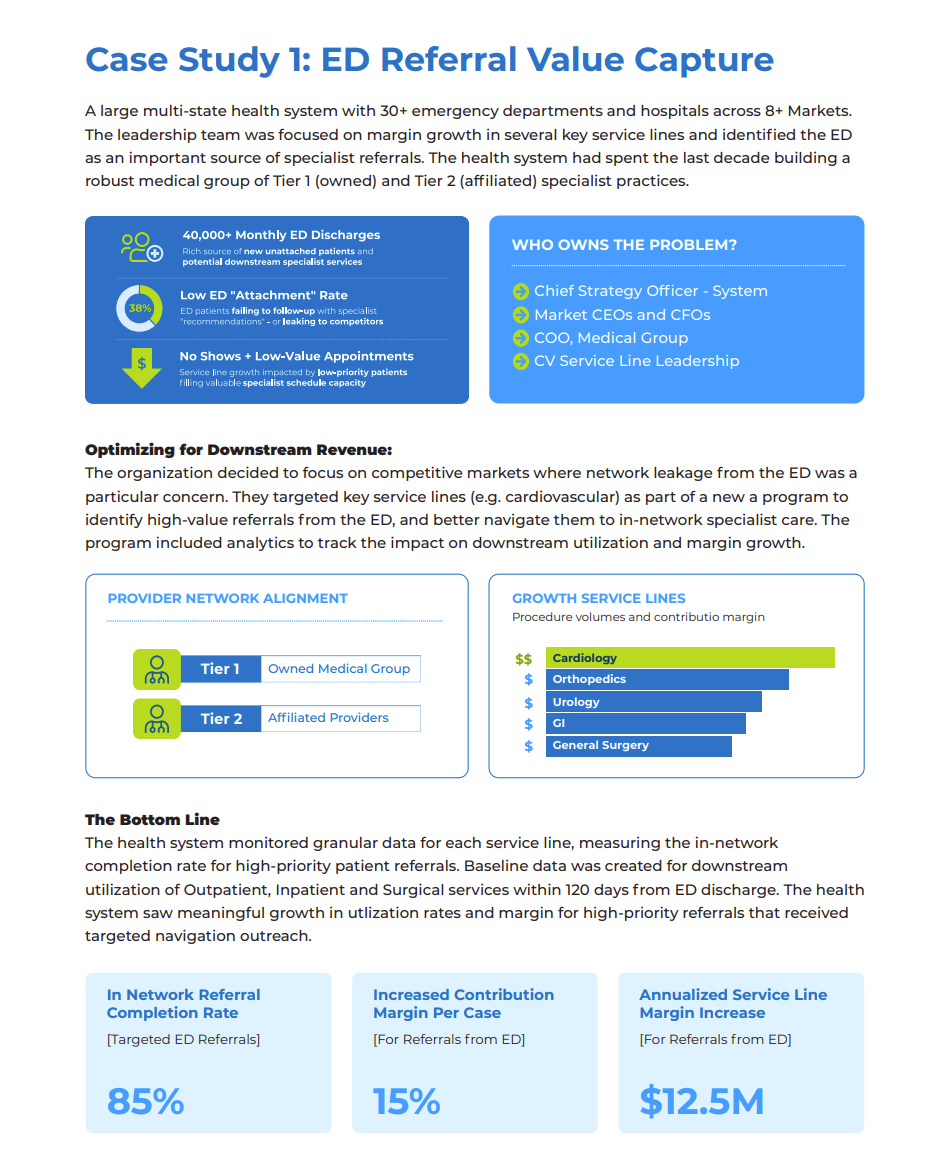
A patient discharged from the ED with a cardiologist referral has a relatively high rate of downstream utilization for outpatient, inpatient, and surgical services.
This metric can be calculated across a population of ED discharges and represented as an average downstream utilization/margin metric to quantify the average value of each cardiology referral.
Keeping more of these patients in the health system network is an obvious benefit – and reducing network leakage, especially for high-value referrals with a high average downstream utilization rate, can be worth millions to the bottom line of that cardiology service line.
-
REQUEST THE FULL BUSINESS CASE
-
GET A DETAILED FINANCIAL MODEL
